Second Trimester Screening (STS) Guide
Second Trimester Screening (STS) is a screening test for trisomy 21 and trisomy 18 consisting of bloodwork in the second trimester of pregnancy. This test is offered to individuals who missed the time window for enhanced First Trimester Screening (eFTS) or if a nuchal translucency (NT) ultrasound is not available in their area.
Step-by-step instructions are outlined below, to provide guidance to health-care practitioners for how to order this test in Ontario.
Maternal Serum Screening (MSS) has been renamed “Second Trimester Screening” or STS. This change applies to the name only to improve understanding of when in pregnancy this screening can be done; the timing and analytes for this screen remain unchanged.
Maternal serum alpha-fetoprotein (MS-AFP) is no longer necessary to routinely screen for open neural tube defects (ONTD), unless there is a barrier to a good quality ultrasound examination.
Step 1 |
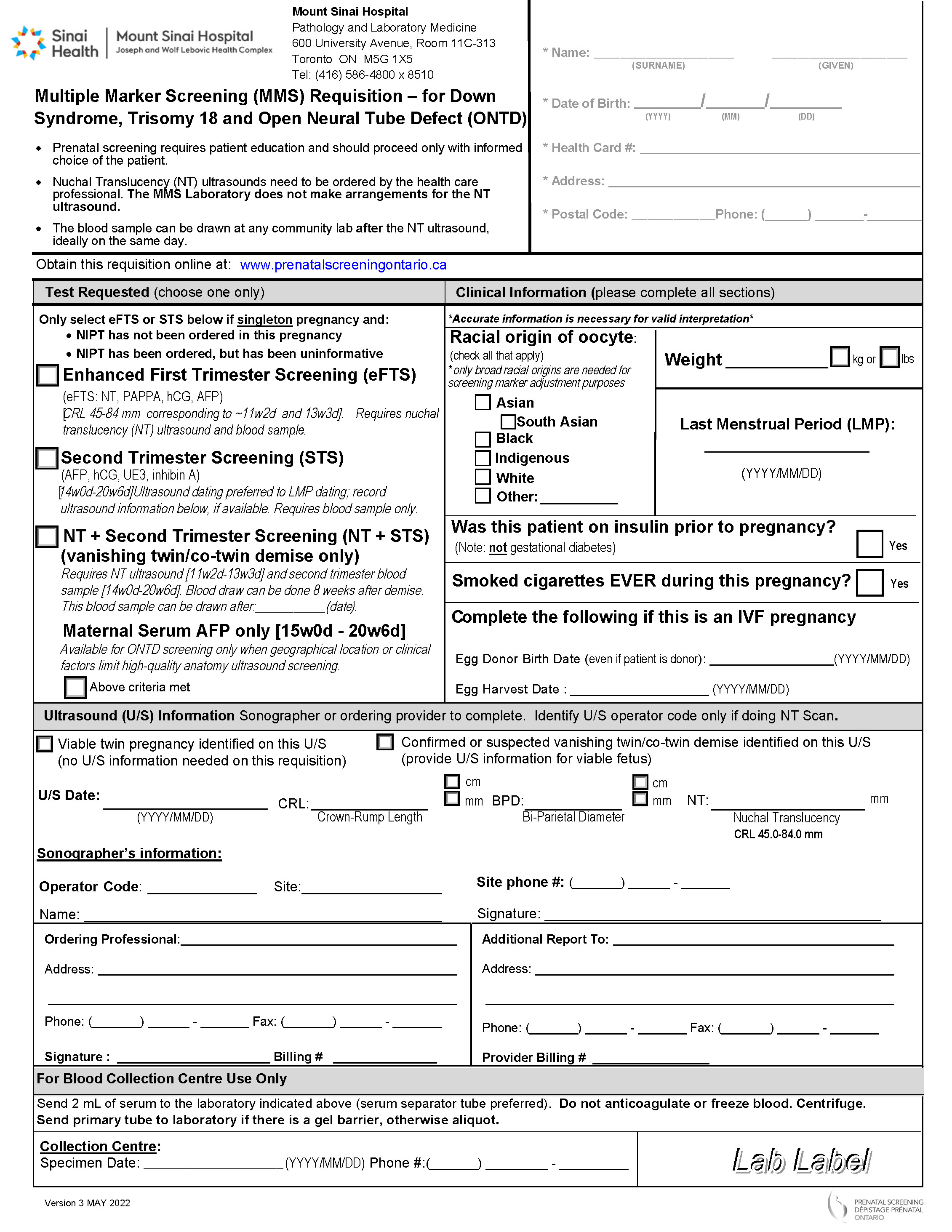
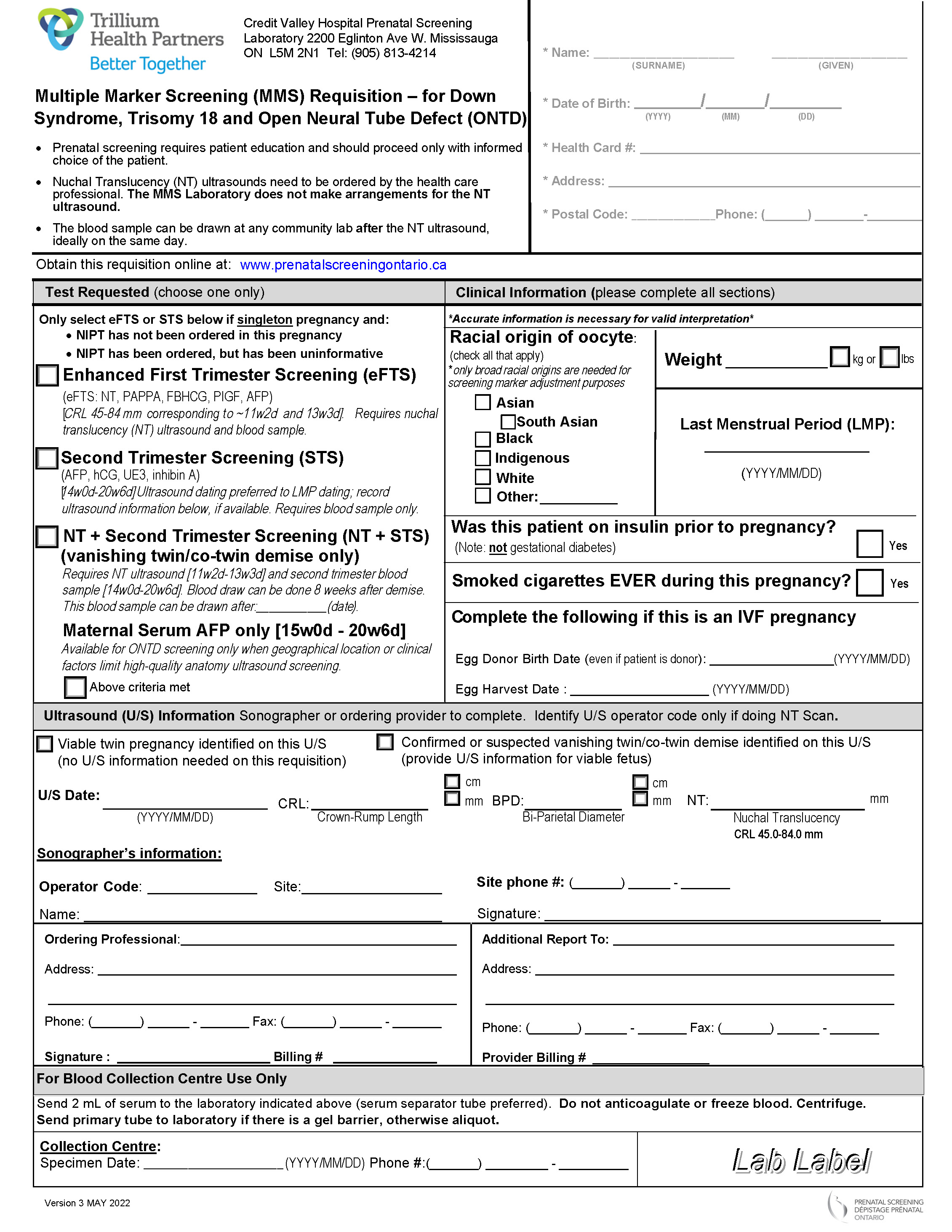
Complete the Multiple Marker Screening Requisition
Multiple Marker Screening (MMS) is done by three provincial laboratories: Trillium Health Partners - Credit Valley Hospital, Mount Sinai Hospital and North York General Hospital. Check out our interactive map to learn which of the three requisitions you should use.
Demographics Section
Document the pregnant individual’s name, date of birth, health card number, address, and phone number.
"Test Requested" Section
Check off the Second Trimester Screening (STS) option only for:
- Singleton pregnancies, with or without vanishing twin/co-twin demise. In a vanishing twin / co-twin demise scenario, note that blood draw must be done at least 8 weeks after the demise of the twin. STS cannot be done for viable twin pregnancies; offer OHIP-funded NIPT instead.
- Pregnancies that are in the gestational time window of 14 weeks 0 days to 20 weeks 6 days. The gestational age is determined either by ultrasound or LMP. Ultrasound is the preferred method of dating.
- Pregnancies for which NIPT has not been ordered.
- Pregnancies for which NIPT has been ordered, but has been uninformative.
"Clinical Information" Section
Accurate and complete information in this section will increase the quality of the screening results by reducing the chance of false positives and false negatives.
I have some questions about you to ask to make sure your screening is as accurate as possible.
| Racial Origin |
|
Indicate the racial origin of the pregnant individual. Racial origin information is needed because the concentrations of screening markers have been shown to vary depending on the racial origin. Therefore, a pregnant individual’s screening markers are adjusted based on the racial origin information provided. Only the broad racial origins listed are needed for screening marker adjustment. The categories on this requisition are not inclusive of the race categories commonly used as social descriptors in Ontario. Description / examples for each of the racial origin categories on the requisition:
Racial origin should be as accurate as possible and should reflect the individual’s ancestral background (which may or may not align with how the pregnant individual identifies), not simply their birth country. This information should be obtained directly from the pregnant individual whenever possible.
|
| Weight |
|
Indicate the pregnant individual’s weight, including units (pounds (lbs) versus kilograms (kg)), at the time when this requisition is completed. This information is used for screening marker adjustments. A weight discrepancy of 10 or more pounds (4.6 kilograms) has a significant impact on the risk for trisomy 21 for pregnant individuals with a risk close to the screening cut-off.
|
| Last Menstrual Period |
|
Indicate the first day of the pregnant individual's Last Menstrual Period (LMP). In the absence of valid ultrasound information, this information will be used to establish the gestational age of the pregnant individual. |
| Insulin-Dependent Diabetes Mellitus History |
|
Indicate if insulin-dependent Diabetes Mellitus was diagnosed prior to the individual’s current pregnancy. Individuals with insulin-dependent Diabetes Mellitus have been shown to have different concentrations of screening markers compared to those who do not have this diagnosis. Screening marker adjustments must be made to account for these differences. No screening marker adjustments are made for pregnant individuals with a history of gestational diabetes or preexisting diabetes that is not managed with insulin.
|
| Cigarette Smoking / Vaping History |
|
Indicate if the pregnant individual has smoked or vaped any amount of nicotine at any point in the current pregnancy. Individuals with a history of smoking or vaping nicotine have been shown to have different concentrations of screening markers compared to those who do not have this history. Screening marker adjustments must be made to account for these differences. If the requisition does not include information about the smoking or vaping history, the pregnant individual is considered a non-smoker. Due to lack of published data, pregnant individuals exposed to second-hand smoke are considered non-smokers.
|
| In Vitro Fertilization (IVF) History |
|
If the pregnancy was conceived using in vitro fertilization (IVF), indicate the egg harvest date and date of birth of the egg donor (either self or non-self). If the egg donor's full date of birth is unknown, indicate the year of birth. If only the year of the donor date of birth is provided, July 1 of the provided year is used as the date. This information is requested because the age of the egg at the date of delivery influences the screening risk. In addition, screening marker levels vary between IVF and natural conceptions and screening marker adjustments must be made to account for these differences.
|
"Ultrasound Information" Section
Be aware that for STS, you, as the ordering health-care practitioner, fills out this section of the requisition. If available, record ultrasound information. Although ultrasound is not required, it is recommended that it is done prior to STS whenever possible. Ultrasound establishes the gestational age more accurately than LMP, and determines the number of fetuses, therefore improving the quality of the screen.
Step 2 |
Provide Requisitions to the Pregnant Individual
-
Give the completed Multiple Marker Screening requisition to the pregnant individual.
- Check if additional requisitions are required by the ultrasound and blood work facilities, such as the Ministry of Health and Long Term Care Laboratory Requisition.

Step 3 |
Provide Step-by-Step Instructions to the Pregnant Individual
Provide the pregnant individual with instructions for how to get STS. Confirm that the pregnant individual is aware of the time window when STS can be done and that the blood draw can be performed at any hospital or community blood collection laboratory.

Step 4 |
Obtain Report and Check for Accuracy
- Results are reported to you by the MMS lab generally within 5 business days. It is important to take into account the time lag that can occur between the time when the report is ready and when it is received by your office.
- If you do not receive the prenatal screening report, we encourage you to follow up with the MMS lab directly. Prenatal Screening Ontario does not have access to screening results of individuals.
- Review the screening report for accuracy. If any errors or omissions are noted, contact the MMS Laboratory to determine if an amendment to the report is needed.
When is a Report Amended?
A report is considered “amended” if changes are made after the report has been issued to the health-care provider. Amending reports is necessary to correct errors that include data being inaccurately provided on the requisition.
It is ideal that gestational age information from a dating ultrasound is used on the MMS requisition (instead of the LMP). Sometimes, the ultrasound information is not included, or the ultrasound occurs after the report is already issued. Amendment of gestational age is made only if the gestational age derived from an ultrasound is found to differ by 10 days or more from the gestational age determined by LMP.
Other indications for amendment are inaccurate racial origin identification, inaccurate diabetes status, and correction of weight, due to either wrong units (i.e. pounds or kilograms) or difference in weight of more than 5 - 10 pounds (2.3 - 4.6 kilograms)1 from that given on the requisition.
1North York General Hospital and Mount Sinai Hospital labs will amend a report if there is a difference in weight of more than 10 pounds. The Trillium Health Partners lab will amend a report if there is a difference in weight of more than 5 pounds.
How is a Report Amended?
Health-care practitioners can write the amendment(s) directly on the screening report and fax it back to the Multiple Marker Screening Laboratory, indicating that an amendment is required as per the enclosed report. Alternatively, health-care practitioners can fax a note with the pregnant individual's name, date of birth, health card number, and details related to the amendment request including relevant clinical information.
Step 5 |
Communicate Results and Next Steps
- Once the report is received, results should be communicated to the pregnant individual in both “screen positive” and “screen negative” scenarios, including the specific risk estimate provided on the report.
- Ensure continuity of care: forward the report to any other practitioners involved in the care of the pregnant individual.


 Subscribe to this page
Subscribe to this page